USF Infectious Diseases Fellows, From Left to Right: Dr. Vidhya Sabapathy, Dr. Ju Hee Katzman, Dr. Greg Teo, Dr. Carlos Lopez-Perez, and Dr. Andrew Nguyen
USF’s Infectious Diseases fellows and faculty were well-represented at the Infectious Diseases Society of America’s annual IDWeek ’19 session, held in Washington, D.C., from October 2 to 6, 2019. USF’s ID Division was collectively responsible for 14 poster presentations displayed between October 3rd through the 5th, and USF ID faculty Associate Professor Dr. Jamie Morano presented in a symposium on her experience in crafting the James A. Haley VA hospital’s outstanding ID Telehealth program, a national leader in the VA system.
A selection of the diverse poster sessions that were presented appears below:
Author and second-year ID fellow Ju Hee Katzman and her co-authors shared data on a series of 38 breast cancer patients who developed gram-negative skin and soft tissue infections following tissue expander surgery. The three most common pathogens found were Pseudomonas aeruginosa, Serratia marcescens, and Klebsiella pneumoniae. They concluded that in centers with a high percentage of gram-negative rods skin and soft tissue infections following tissue expander surgery, treating physicians should consider using perioperative antibiotics that include coverage against Pseudomonas, the most common isolate (45%).
Former (2017-2019) infectious disease fellow Dr. Shylah Moore and colleagues presented a poster on a five-year retrospective review within Florida’s Hillsborough County Department of Health comparing the trends and outcomes among HIV infected versus HIV uninfected patients with tuberculosis. Results suggested an HIV-TB coinfection rate that is slightly higher than the national population, with co-infected patients in the study sample having a statistically significant higher rate for cavitary TB.
Dr. Vidhya Sabapathy in front of her poster
Second year fellow Dr. Vidhya Sabapathy and colleagues reported on a retrospective analysis of 61 adult patients between 2010 and 2018 who were diagnosed and being treated for acute leukemia. All of the selected patients experienced severe neutropenia for 7 days or greater. Patient characteristics and infectious complications were examined. The most common diagnosis was AML. Bloodstream infections were the most common site, followed by respiratory tract infections. Gram-positive organisms were the leading etiology of bacteremias. In the subset of patients undergoing multiple induction chemotherapy, gram-negative pathogens were the leading cause of the bloodstream infections.
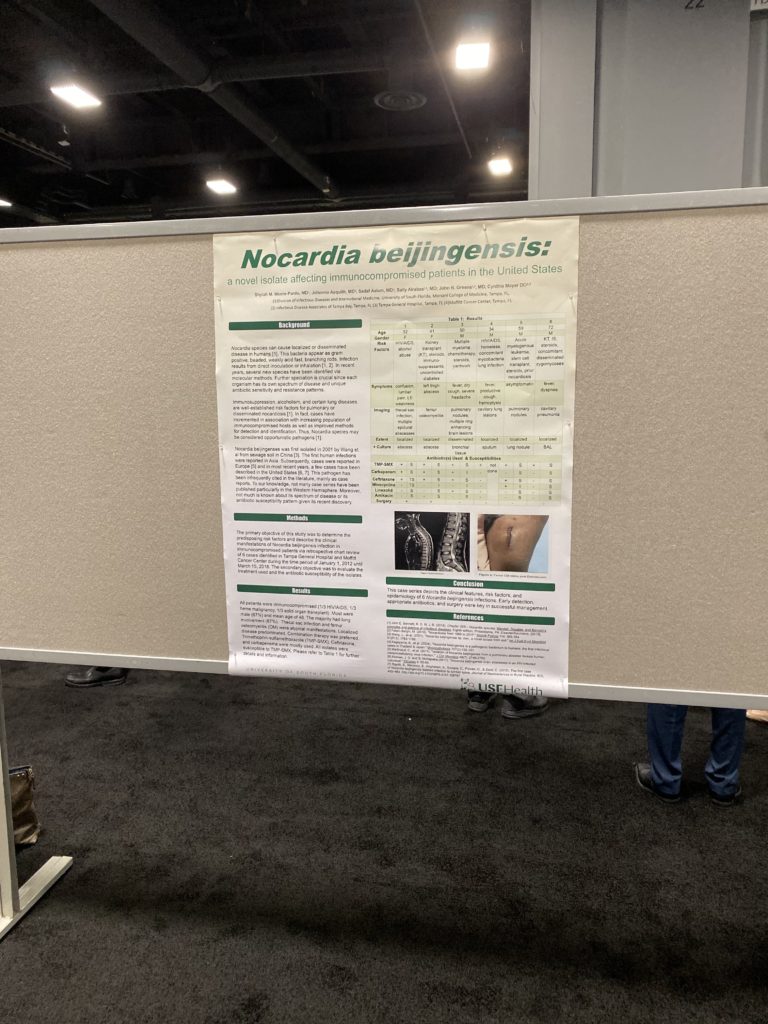
Dr. Shylah Moore and Colleagues’ Poster on Nocardia beijingensis
Dr. Shylah Moore, Dr. Johanna Asquith, and colleagues also reported on a retrospective chart review of 6 cases of a more recently described Nocardia strain first isolated in 2001 from sewage soil in China. The purpose of the study was to determine the risk factors and clinical manifestations of Nocardia beijingensis infection. All of the cases reviewed involved immunocompromised patients, were predominantly male, and had a mean age of 48. Most had lung involvement. Atypical manifestations included thecal sac infection and femur osteomyelitis. All isolates were susceptible to trimethoprim/sulfamethoxazole, but ceftriaxone and carbapenems were mostly used.
Dr. Carlos Perez-Lopez, a second year infectious diseases fellow and other co-authors reviewed a retrospective cohort of patients for seropositivity to Strongyloides stercoralis who underwent transplant evaluation from 2014-2016. A total of 228 charts were reviewed, and 113 seropositive patients were identified. Male gender and caucasian race predominated in both the seronegative and seropositive groups. The study did not find any statistically significant difference in the demographic characteristics or risk factors that can be used for prediction of Strongyloides seropositivity among solid organ transplant candidates. Thus, the validity of universal screening was reinforced.
Dr. Jamie Morano, far left, on the panel at “Success Stories in Telehealth.”
Dr. Jamie Morano presented as part of the symposium, “Success Stories in Teleheath,” on “ID Telehealth Best Practices: Veterans Administration.” She presented with Christopher Crnich, MD, and Rima Abdel-Massih, MD, with Moderator John Lynch, MD, also on the podium.
For more information about IDWeek’s 2019 Scientific program, please visit the interactive program page.